Ushering in the Second Wave of Checkpoint Blockade Therapies
Immune checkpoint blockade has emerged over the past decade as a useful therapeutic tool against many types of tumors. Checkpoint blockade therapies take advantage of the fact that many tumors are infiltrated by immune cells, but those cells are unable to effectively kill the tumor due to inhibitory signals that limit their function. By reversing inhibitory signals that block T cell functionality, checkpoint blockade therapy reactivates immune cells already in a tumor and allows them to resume their effector function1.
The most commonly known checkpoint that can be targeted therapeutically is the PD-1/PD-L1 pathway. In fact, FDA approval for several drugs targeting this pathway took place in 20172. PD-1 is a receptor found on T cells, and is upregulated on “exhausted” T cells that have seen chronic antigen stimulation3. Because tumors are an antigen-rich environment, tumor-infiltrating T cells, or TIL, often and rapidly begin to upregulate PD-1. Many tumor cells express PD-L1 on their cell surface4,5. Interaction between PD-L1 and PD-1 expressed on T cells leads to the transmission of a regulatory signal to the T cells6. Therefore, blocking the interaction between PD-1 and PD-L1 increases the effector function of TIL and lead to an anti-tumor immune response that extends progression-free and overall survival in a subset of cancer patients7.
Following the success of anti-PD-(L)1 therapy, several emerging checkpoint inhibitors have been tested in model systems. Signaling through these pathways confers a similar inhibitory effect on T cells to that downstream of PD-1. LAG-3, BTLA, TIM-3, and TIGIT are some of the receptors that T cells use to downregulate their response to antigen and have been proposed as novel therapeutic targets, and several recent reviews highlight the potential of these novel checkpoint targets8,9. The ligands to these receptors can be found, similarly to PD-L1, on the surface of tumor cells and/or antigen presenting cells, meaning that inhibition of TIL via these signaling pathways is expected to occur within tumors. Indeed, patent applications have already been filed around the world for targeting these receptors therapeutically9.
One major reason for the continuing development of novel checkpoint blockade immunotherapies is that only a fraction of patients respond to PD-(L)1 or CTLA4 blockade, and resistance to these therapies can develop in patients that do initially present with a response10,11. Some patients, for example, decrease expression of specific checkpoint markers in a biologic escape mechanism to these therapies, but other molecules with similar cellular functions could still be targeted to achieve similar effects12. As a new wave of immunotherapies makes its way through the pipeline, this is an exciting time to see the growing potential of targeting so many components of the immune system to treat cancer.
Comparing Bethyl antibodies to competitors'
Bethyl's new PD-L1 recombinant rabbit monoclonal antibody was compared against the leading competitor's antibody and proved to be 8 times more sensitive. Antibodies were tested in accordance to each manufacturer's protocol as stated on the product datasheet, which seeks to optimize antibody performance.
Leading Competitor's Rabbit anti-PD-L1 Monoclonal Antibody
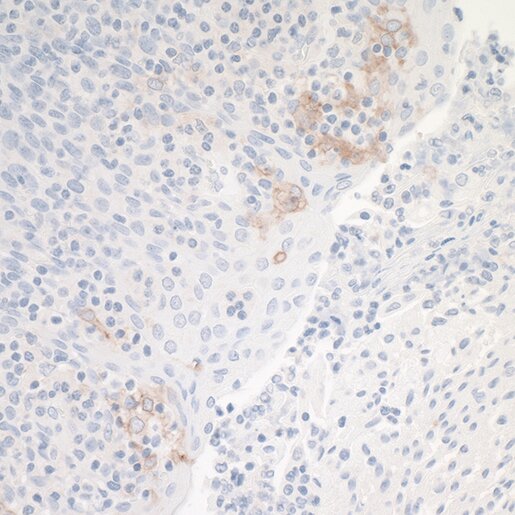
Application: IHC • Sample: Tonsil
Bethyl's Rabbit anti-PD-L1 Recombinant Monoclonal Antibody [BLR020E] (A700-020)
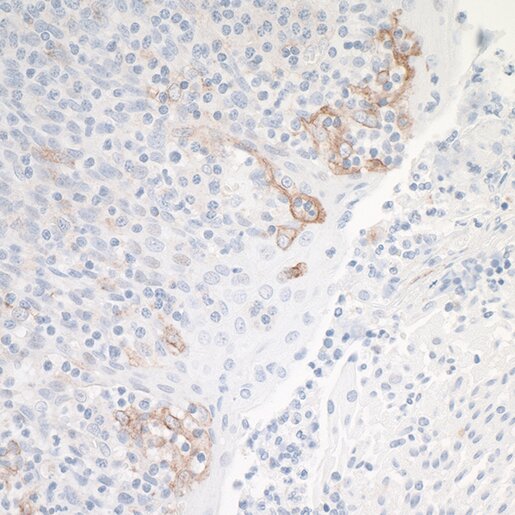
Application: IHC • Sample: Tonsil
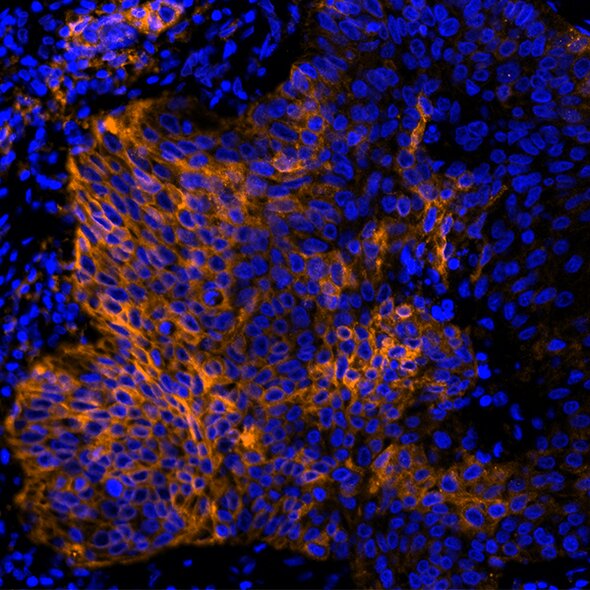
Detection of human PD-L1 (orange) in FFPE lung carcinoma by IHC-IF (pseudo color). Antibody: Rabbit anti-PD-L1 recombinant monoclonal [BLR020E] (A700-020). Secondary: DyLight® 594-conjugated goat anti-rabbit IgG (A120-201D4). Counterstain: DAPI (blue).
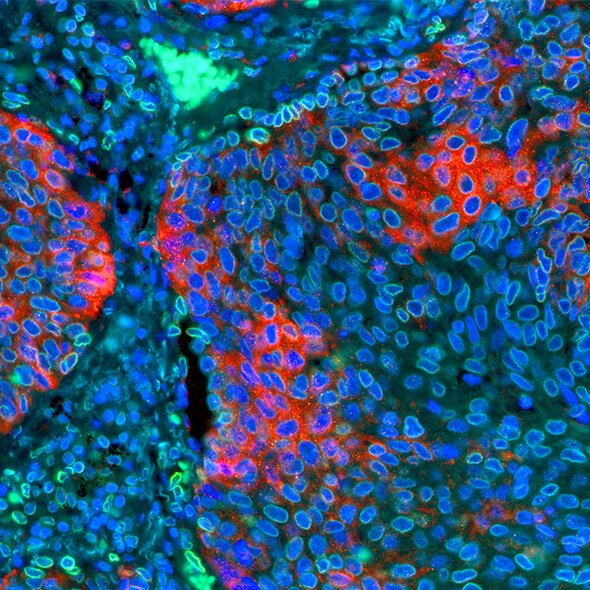
Detection of human PD-L1 (red) and Lamin-A/C (green) in FFPE lung by IHC-IF. Antibody: Rabbit anti-PD-L1 recombinant monoclonal [BLR020E] (A700-020) and rabbit anti-Lamin-A/C (A303-430A). Secondary: DyLight® 594-conjugated goat anti-rabbit IgG (A120-201D4) and DyLight® 488-conjugated goat anti-rabbit IgG (A120-201D2). Counterstain: DAPI (blue).
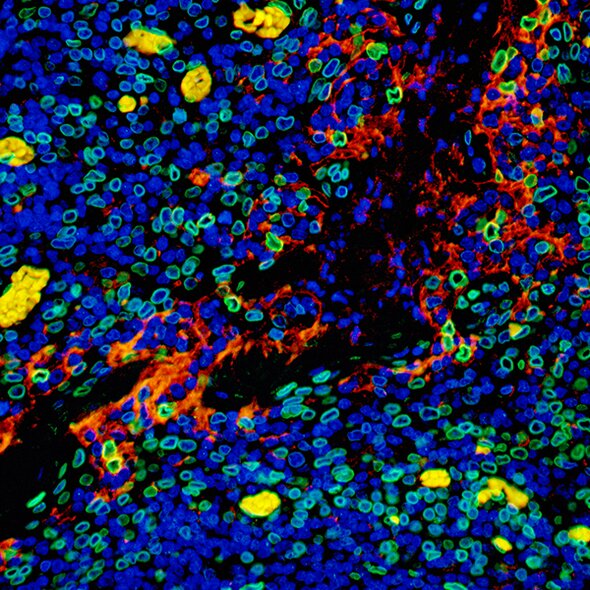
Detection of human PD-L1 (red) and Lamin-A/C (green) in FFPE tonsil by IHC-IF. Antibody: Rabbit anti-PD-L1 recombinant monoclonal [BLR020E] (A700-020) and rabbit anti-Lamin-A/C (A303-430A). Secondary: DyLight® 594-conjugated goat anti-rabbit IgG (A120-201D4) and DyLight® 488-conjugated goat anti-rabbit IgG (A120-201D2). Counterstain: DAPI (blue).
References
- Zhou G, Sprengers D, Boor PPC, et al. 2017. Antibodies Against Immune Checkpoint Molecules Restore Functions of Tumor-Infiltrating T Cells in Hepatocellular Carcinomas. Gastroenterology. Oct;153(4):1107-1119.e10. doi:10.1053/j.gastro.2017.06.017.
- Gong J, Chehrazi-Raffle A, Reddi S, Salgia R. 2018. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J Immunother Cancer. Jan 23;6(1):8. doi:10.1186/s40425-018-0316-z.
- Blackburn SD, Shin H, Freeman GJ, Wherry EJ. 2008. Selective expansion of a subset of exhausted CD8 T cells by PD-L1 blockade. Proc Natl Acad Sci. Sept 30;105(39):15016-15021.
- Badalamenti G, Fanale D, Incorvaia L, et al. 2018. Role of tumor-infiltrating lymphocytes in patients with solid tumors: Can a drop dig a stone? Cell Immunol. Jan 30. doi:10.1016/j.cellimm.2018.01.013.
- Gatalica Z, Snyder C, Maney T, et al. 2014. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev. Dec;23(12):2965-2970.
- Jin H-T, Ahmed R, Okazaki T. 2010. Role of PD-1 in Regulating T-Cell Immunity. In: Vol Springer, Berlin, Heidelberg:17-37.
- Dong Y, Sun Q, Zhang X. 2017. PD-1 and its ligands are important immune checkpoints in cancer. Oncotarget. Jan 10;8(2):2171-2186.
- Torphy RJ, Schulick RD, Zhu Y. 2017. Newly Emerging Immune Checkpoints: Promises for Future Cancer Therapy. Int J Mol Sci. Dec 6;18(12). doi:10.3390/ijms18122642.
- Collin M. 2016. Immune checkpoint inhibitors: a patent review (2010-2015). Expert Opin Ther Pat. May;26(5):555-564.
- Jenkins RW, Barbie DA, Flaherty KT. 2018. Mechanisms of resistance to immune checkpoint inhibitors. Br J Cancer. Jan;118(1):9-16.
- Bai J, Gao Z, Li X, Dong L, Han W, Nie J. 2017. Regulation of PD-1/PD-L1 pathway and resistance to PD-1/PD-L1 blockade. Oncotarget. Nov 25;8(66):110693-110707.
- Nirschl CJ, Drake CG. 2013. Molecular pathways: coexpression of immune checkpoint molecules: signaling pathways and implications for cancer immunotherapy. Clin Cancer Res. Sept 15;19(18):4917-4924.